12 Sep From MMJ to Special K
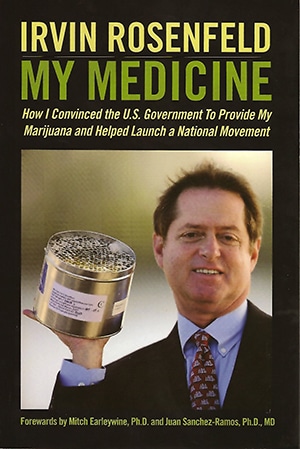
Every five months Irvin Rosenfeld gets a FedEx shipment, courtesy of the federal government, containing six metal canisters, each with 300 perfectly rolled joints of what today would be considered rather mediocre weed. But the quality of the government-issue reefer matters less than the fact that Uncle Sam has been supplying him with it regularly since 1982, when Rosenfeld won the right to smoke cannabis for reasons of medical necessity under the auspices of the federal government’s Compassionate Investigational New Drug (IND) program. Rosenfeld smokes cannabis every day to treat a rare and excruciatingly painful bone disease called multiple congenital cartilaginous exotosis.
Medicine in a Can

A total of 15 patients with different incurable ailments would enroll in the Compassionate IND Program to study cannabis before it was officially shut down in 1992. As one of the last living IND participants, Rosenfeld remains a forthright and energetic medical cannabis advocate, a role he takes very seriously. His personal story is compelling. He has suffered with extreme pain for most of his life. At age 10, x-rays revealed more than 200 tumors sprouting from bones in his arms and legs. He would undergo a dozen surgeries and consume a steady diet of prescription narcotics and other pharmaceuticals.
When he first smoked marijuana as a teenager at a social gathering, it was a revelation. Before long he realized that if he smoked cannabis every couple of hours, his pain eased and he didn’t have to rely as much on doctor-prescribed muscle relaxants, opiates, and benzos to get by. Although he felt no euphoric effects from cannabis, the herb somehow kept his disease in check, inhibiting tumor growth and helping him live a decent life. A walking, talking refutation of the lazy stoner myth, he went to college, played sports, married his childhood sweetheart Debbie, and became a successful stockbroker.
There’s no doubt that cannabis helps Rosenfeld’s condition, but it’s not a cure. Though he has learned to live with his pain, at times its relentlessness makes him feel depressed, trapped in a lonely prison from which there’s no escape. At least that’s how it felt until one day in 2020, when Rosenfeld’s pain management specialist, Dr. Michele Weiner, mentioned a potential jailbreak: ketamine.
Dissociation Nation
Ketamine, an FDA-approved “dissociative anesthetic,” has been around since 1962 when it was first synthesized by chemist Calvin Stevens. Employed initially as a tranquilizer in veterinary medicine, the drug was widely utilized during the Vietnam War for treating wounded troops. Ketamine kept injured soldiers conscious but cognitively disconnected from their pain, all while maintaining their vital functions.
Ketamine’s efficacy against pain is attributed to the drug’s ability to induce a dissociative state. At high doses ketamine produces anesthesia; at lower doses, it relieves pain and causes hallucinations. “Special K” acquired a reputation as a party drug in the 1970s due to its psychedelic and mood-altering effects. Favored by fashionistas and Silicon Valley bros, it’s still part of the recreational drug scene.
Some have attributed Elon Musk’s erratic behavior of late to ketamine benders at parties. (He says he uses it to relieve depression — proof that money can’t buy everything.) Although ketamine is potentially addictive and excessive use can cause liver damage, renal failure, and psychotic episodes, it’s classified as a Schedule III controlled substance (along with anabolic steroids and some acetaminophen-codeine combinations), indicating a relatively low risk for abuse.
Unlike LSD and psilocybin, ketamine has no natural source. Lysergic acid is present in ergot (rye fungus), psilocybin is a magic mushroom compound, mescaline comes from the peyote cactus, and for MDMA (“ecstasy”) there’s sassafras. But there’s no natural correlate for synthetic ketamine, which works through different molecular pathways than the classic, naturally sourced psychedelics. Acid and ‘shrooms deliver a full-blown psychedelic experience by binding to the 5-HT2A serotonin receptor, whereas ketamine confers its powerful dissociative and psychedelic effects by blocking the N-methyl-d-aspartate (NMDA) receptor, a glutamate ion channel that manages the ebb and flow of calcium inside the cell.
Fertilizer for the Brain
By inhibiting the NMDA receptor, ketamine triggers the production of a chemical known as brain-derived neurotrophic factor (BDNF), which has been likened to “fertilizer of the brain.” The role of BDNF in adult neurogenesis (the creation of new brain cells) and neuroplasticity (the ability to reorganize neural networks and synaptic connections in response to injury and lived experience) is the subject of many scientific papers.
According to a 2012 study by University of Bonn scientist Andras Bilkei-Gorzo: “On the cellular level, the cannabinoid system regulates the expression of brain-derived neurotrophic factor and neurogenesis.” Subsequent reports by Brazilian investigators established that ketamine’s central and peripheral painkilling effects are mediated by the endocannabinoid system. When scientists blocked the CB1 cannabinoid receptor, ketamine did not prevent pain. The same group of researchers also found that ketamine caused anandamide (one of two major endocannabinoids) to be released in certain brain areas. And when anandamide levels increased, so did ketamine’s analgesic effect.
Plant cannabinoids have also been shown to potentiate ketamine’s painkilling properties. A 2011 report on “The interplay of cannabinoid and NMDA glutamate receptor systems” examined “the interactive effects of cannabidiol and ketamine in healthy human subjects.” The report concluded that “CBD significantly augmented the activating effects of ketamine.” Other studies have noted that CBD boosts endocannabinoid levels and CB1 receptor signaling by delaying the metabolic breakdown and reuptake of anandamide.
CBD and ketamine are both neurogenic compounds, and this may factor into how they confer antidepressant effects. Impaired neurogenesis has been linked to clinical depression, substance abuse, and other mental health conditions. Ketamine’s rapid antidepressant effects involve enhanced BDNF-induced (and cannabinoid-regulated) neurogenesis and neuroplasticity. The drug is currently being administered off-label for refractory depression at numerous ketamine clinics around the country.
Common Biological Mechanisms
“Pain and depression share common biological mechanisms,” explains Dr. Michelle Weiner, a double board-certified physician who specializes in interventional pain medicine, physical medicine, and rehabilitation. In addition to her clinical practice at five locations in southern Florida, Dr. Weiner is an Assistant Professor at Nova Southeastern University College of Osteopathic Medicine.
Take a spin on her website and you’ll find a group photo picturing Dr. Weiner and her team of practitioners, a bevy of Florida beauties who look as though they could’ve been cast as the Real Housewives of Miami. There’s a lot going on behind the glamor. When interviewed by Project CBD, Dr. Weiner’s enthusiasm for her calling is obvious, her expertise backed by years of on-the-ground research and a vast knowledge rooted in pain studies and cutting-edge neuroscience.
While building her practice, Dr. Weiner grew increasingly frustrated with the limited tools available beyond conventional pain pills and injections. When medical cannabis was legalized in Florida in 2016, she became one of the first licensed physicians to include it in her treatment plans. She found that cannabis was an effective therapeutic option for helping chronic pain patients, especially seniors, decrease their dependence on opioids.
“It really changed my practice,” says Weiner, who is a member of Florida’s Medical Cannabis Advisory Committee. Weiner’s experience as a cannabis clinician encouraged her to explore other mind-body healing modalities, including psychedelic drugs. Today she is vice president of Mr. Psychedelic Law, a not-for-profit that advocates for responsible legal reform of psilocybin prohibition in the Sunshine State.
Teaching Resilience
Dr. Weiner’s interest in ketamine began during a residency and training fellowship at the University of Miami. “Back then we used ketamine differently than we do now,” she says. “We’d give patients a benzodiazepine sedative beforehand to tone down the hallucinatory experiences common with ketamine.” But after learning of ketamine’s potential as treatment for anxiety, depression, and PTSD, she changed her approach to encompass a dual-pronged focus on pain and mental health.
“Eighty-five percent of chronic pain patients also suffer from depression,” says Dr. Weiner. “You can’t successfully treat pain without concurrently treating mental health.” From her perspective, it’s all interconnected: chronic pain adversely impacts how the brain functions, causing maladaptive changes in the central nervous system and weakening synaptic circuitry between brain regions — and these changes often lead to depression, according to a 2017 study published in the journal Neural Plasticity. Not only does it offer rapid relief from both depression and pain, ketamine also appears to refresh and reset neural circuitry.
But the benefits of a single ketamine treatment are often short-lived (seven days on average for depression), and the drug may be contraindicated for certain conditions. Some people can’t tolerate ketamine’s intense hallucinogenic effects. Another major drawback: MediCare and health insurance companies don’t cover ketamine treatments, so patients must pay out of pocket. For those who can’t afford it, there are DIY at-home ketamine kits with medicine procured from less-than-reliable online sources, which is problematic.
Ketamine treatment needs to be monitored by an experienced practitioner, says Dr. Weiner. Most of her patients come into the clinic once or twice a week for at least a month to receive ketamine by intramuscular or intravenous infusion, along with therapy sessions and lifestyle counseling for a better long-term outcome. Treatment is tapered off over time, and the benefits are maintained with occasional ketamine “boosters,” an approach backed by research. The goal is to relieve pain while helping patients learn new strategies for how to live with it.
“When used mindfully,” says Dr. Weiner, “ketamine, through its dissociative effects, allows patients a time-out from their pain. Yes, it’s temporary, but being able to take a break from intense pain also gives them a chance to see it from a different perspective. It’s not who they are. It’s not their identity. Ketamine disrupts the static and unproductive patterns with which patients deal with their pain and encourages the development of better life strategies. What we’re really doing is teaching them resilience.”
A Remarkable Drug
Unlike Dr. Weiner’s other patients, Irv Rosenfeld has her blessing to treat himself orally with ketamine at his own home. The fact that she makes an exception in Irv’s case is a testament to her admiration and respect for Rosenfeld, who has been under Dr. Weiner’s pain management care for many years.
Every five days or so, when the pain in his bones gets really bad, Irv texts his wife Debbie before he drives home from work: I’m doing ketamine tonight. Debbie knows to stay close by yet out of his way. In order to “do ketamine,” Rosenfeld needs complete isolation and quiet. Once at his house in Fort Lauderdale, he will put on some classical music. Then he’ll place one-and-a-half sublingual tablets containing a total of 300 milligrams of ketamine between his cheek and gum, sit down in a comfortable armchair, and wait for the portal to open. His flight from pain is about to take off.
About an hour passes before Rosenfeld notices any effects. When they arrive, the feelings are both physical and emotional. He can see “the pain flow out and float far away,” he tells Project CBD. Under the influence of “forgetamine,” existential agony and exhaustion are replaced by euphoric hallucinations lasting several hours with his eyes closed.
Rosenfeld accepts that the relief he gets from ketamine won’t last beyond his solitary, three-to-four-hour sit-down sessions. But the knowledge that he can occasionally be whisked away from the Land of Pain is in and of itself transformative, nourishing his innate resilience and helping him tackle life’s daily challenges.
“It’s a remarkable drug,” he says with an obvious tone of gratitude. Just as pain has influenced the course of Rosenfeld’s life, so has his outspoken activism, his efforts to get the word out about the therapeutic benefits of cannabis before most people knew much about it. And now he’s also singing the praises of ketamine. Listening to him talk is uplifting, like getting a dose of medicine you really need.
Melinda Misuraca is a Project CBD contributing writer with a past life as an old-school cannabis farmer specializing in CBD-rich cultivars. Martin A. Lee is the director of Project CBD. He’s authored and edited several books, including Smoke Signals, Acid Dreams, and The Essential Guide to CBD. © Copyright, Project CBD. May not be reprinted without permission.
Sources
- Bilkei-Gorzo A. The endocannabinoid system in normal and pathological brain ageing. Philos Trans R Soc Lond B Biol Sci. 2012 Dec 5;367(1607):3326-41. doi: 10.1098/rstb.2011.0388. PMID: 23108550; PMCID: PMC3481530.
- Duman RS, Aghajanian GK, Sanacora G, Krystal JH. Synaptic plasticity and depresson: new insights from stress and rapid-acting antidepressants. Nat Med [Internet]. 2016;22(3):238–49.
- Ferreira RCM, Castor MGM, Piscitelli F, Di Marzo V, Duarte IDG, Romero TRL. The Involvement of the Endocannabinoid System in the Peripheral Antinociceptive Action of Ketamine. J Pain. 2018 May;19(5):487-495. doi: 10.1016/j.jpain.2017.12.002. Epub 2017 Dec 13. PMID: 29247851.
- Hallak JE, Dursun SM, Bosi DC, de Macedo LR, Machado-de-Sousa JP, Abrão J, Crippa JA, McGuire P, Krystal JH, Baker GB, Zuardi AW. The interplay of cannabinoid and NMDA glutamate receptor systems in humans: preliminary evidence of interactive effects of cannabidiol and ketamine in healthy human subjects. Prog Neuropsychopharmacol Biol Psychiatry. 2011 Jan 15;35(1):198-202. doi: 10.1016/j.pnpbp.2010.11.002. Epub 2010 Nov 7. PMID: 21062637.
- Khakpai F, Ebrahimi-Ghiri M, Alijanpour S, Zarrindast MR. Ketamine-induced antidepressant like effects in mice: A possible involvement of cannabinoid system. Biomed Pharmacother. 2019 Apr;112:108717. doi: 10.1016/j.biopha.2019.108717. Epub 2019 Feb 28. PMID: 30970516.
- Murrough JW, Perez AM, Pillemer S, Stern J, Parides MK, aan het Rot M, Collins KA, Mathew SJ, Charney DS, Iosifescu DV. Rapid and longer-term antidepressant effects of repeated ketamine infusions in treatment-resistant major depression. Biol Psychiatry. 2013 Aug 15;74(4):250-6. doi: 10.1016/j.biopsych.2012.06.022. Epub 2012 Jul 27. PMID: 22840761; PMCID: PMC3725185.
- Niciu MJ, Henter ID, Luckenbaugh DA, Zarate CA Jr, Charney DS. Glutamate receptor antagonists as fast-acting therapeutic alternatives for the treatment of depression: ketamine and other compounds. Annu Rev Pharmacol Toxicol. 2014;54:119-39. doi: 10.1146/annurev-pharmtox-011613-135950. PMID: 24392693; PMCID: PMC4089991.
- Nutt DJ. Relationship of neurotransmitters to the symptoms of major depressive disorder. J Clin Psychiatry. 2008;69 Suppl E1:4-7. PMID: 18494537.
- Pacheco DDF, Romero TRL, Duarte IDG. Ketamine induces central antinociception mediated by endogenous cannabinoids and activation of CB1 receptors. Neurosci Lett. 2019 Apr 23;699:140-144. doi: 10.1016/j.neulet.2019.01.059. Epub 2019 Feb 1. PMID: 30716423.
- Pourmand A, Mazer-Amirshahi M, Royall C, Alhawas R, Shesser R. Low dose ketamine use in the emergency department, a new direction in pain management. Am J Emerg Med. 2017 Jun;35(6):918-921. doi: 10.1016/j.ajem.2017.03.005. Epub 2017 Mar 2. PMID: 28285863.
- Riccardi A, Guarino M, Serra S, Spampinato MD, Vanni S, Shiffer D, Voza A, Fabbri A, De Iaco F; Study and Research Center of the Italian Society of Emergency Medicine. Narrative Review: Low-Dose Ketamine for Pain Management. J Clin Med. 2023 May 2;12(9):3256. doi: 10.3390/jcm12093256. PMID: 37176696; PMCID: PMC10179418.
- Sheng J, Liu S, Wang Y, Cui R, Zhang X. The Link between Depression and Chronic Pain: Neural Mechanisms in the Brain. Neural Plast. 2017;2017:9724371. doi: 10.1155/2017/9724371. Epub 2017 Jun 19. PMID: 28706741; PMCID: PMC5494581.
- Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018 Apr;23(4):801-811. doi: 10.1038/mp.2017.255. Epub 2018 Mar 13. PMID: 29532791; PMCID: PMC5999402.


Sorry, the comment form is closed at this time.