29 Mar Cancer & the CB2 Receptor
The cannabinoid receptor CB1, primary target of THC in the brain, is known for mediating the cannabis high. And its counterpart CB2, mainly expressed in immune cells throughout the body, is understood to play an important role in inflammatory processes. These abstractions are accurate as far as they go, but as with anything related to the endocannabinoid system, reality is far more complex.
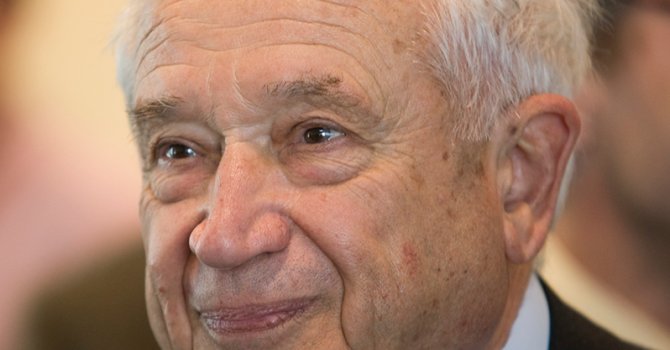
Project CBD’s recent article on the passing of Raphael Mechoulam noted that the esteemed scientist believed CB2 should be a focus of future cannabinoid science. The CB2 receptor interacts with THC, CBD, endocannabinoids, and other compounds in a multitude of organs including skin and bone.
Recent research – including papers co-authored by Mechoulam well into his 80s – has confirmed that aberrant CB2 signaling is implicated in a raft of autoimmune, neurodegenerative, metabolic, and psychiatric disorders. CB2 is also an increasingly hot topic in cancer research.
In this two-part series, Project CBD will explore some of the latest studies and what they reveal about what we know – and still don’t know – about this ubiquitous, somewhat mysterious cell receptor.
This week: cancer. Next week: cognitive and mood disorders, including some of Mechoulam’s final work before his death in March at the age of 92.
Prostate Cancer & a New CB2 Ligand
Three studies from the first few months of 2023 probe the function of CB2 in three different cancer models. While their findings are complex and not necessarily conclusive, they contribute to a growing body of knowledge about the potential efficacy of cannabinoids in cancer treatment.
A paper published in February in the International Journal of Molecular Sciences1 offers two insights for the price of one: first, another look at how the CB2 receptor functions in a cellular model of cancer; and second, new evidence that a compound called 3-3′-Diindolylmethane (DIM) – present in cruciferous vegetables such as cauliflower, cabbage, broccoli, Brussels sprouts, and a number of leafy greens – exerts anti-cancer effects through the CB2 receptor.
By testing DIM on two different human prostate cancer cell lines, the Italy- and UK-based researchers observed that the compound activated naturally expressed CB2 receptors in both lines – and that in one, known as “PC3,” CB2 activation led to cell death, an effect that was reversed when the researchers blocked the CB2 receptor with an antagonist.
DIM was already known to have an anti-cancer effect more broadly. What had not been previously observed, the authors note, is CB2’s role in mediating this effect in a human cancer cell line. “We can conclude that DIM is a CB2 receptor ligand with a potential anti-prostate cancer effect,” they write.
If true, cruciferous vegetables join saffron, black pepper, cloves, oregano, and some other spices as foods containing compounds that interact with the CB2 receptor in beneficial ways.
But don’t head to the market for a cartload of cauliflower and cabbage just yet. The concentrations of DIM used in the study are too high to be obtained through diet alone, the authors note, and administration by supplements may be required.
Colon Cancer: Case Closed?
A second February 2023 study in the International Journal of Molecular Sciences2 comes to a similar conclusion regarding CB2’s role in colon cancer. Researchers in Israel investigated how the CB2 receptor functioned in a mouse model of colon cancer (utilizing “knockout” mice missing the receptor altogether), and they analyzed genomic data in a large human population to determine the relationship between CB2 variants and colon cancer incidence.
In both cases, the authors write, their findings indicate that “endogenous CB2 activation can modulate the immune response and consequently reduce tumorigenesis” and that “CB2 protects against the development of colon cancer.”
Yet despite their seemingly unambiguous findings, the authors also acknowledge that previous studies have come to very different conclusions about the role of CB2 in cancer.
“CB2 has been investigated in multiple cancer types and models of inflammation,” they write, “and there are controversial results regarding the effect on tumor progression.” For example, past studies have found that CB2 expression is associated with a poor prognosis in humans; that CB2 antagonists, or blockers, suppress tumor growth; that CB2 activation promotes tumor growth in models of colon cancer; and that CB2 agonists inhibit tumor growth. The researchers attribute this ambiguity to variations in animal cancer models and cancer cell lines.
Lung Cancer: A Different Answer
Sure enough, a different study published a month earlier in Frontiers in Immunology3 using a different mouse model of non-small cell lung cancer seems to show something else altogether.
Within knockout mice deficient of CB2 in the “tumor microenvironment” – the normal cells, molecules, and blood vessels that surround a tumor cell, including immune cells expressing high levels of CB2 – a team of Austria-based researchers observed a reduction in tumor burden relative to “wild-type” mice. They also found that CB2-deficient mice responded significantly better to a form of immunotherapy known as anti-PD1.
Together, these findings indicate that CB2 receptors in the tumor microenvironment of non-small cell lung cancer “may act as an immunosuppressor … thereby promoting tumor growth.”
You read that right: the opposite of what the other two papers found. Be that as it may, it still seems clear enough that CB2 modulates cellular immune response in ways directly relevant to cancer progression – and that the clinical implications of this link still need to be worked out.
Nate Seltenrich, an independent science journalist based in the San Francisco Bay Area, covers a wide range of subjects including environmental health, neuroscience, and pharmacology. Copyright, Project CBD. May not be reprinted without permission.





Sorry, the comment form is closed at this time.